Acute myocarditis is one of those diseases that is a catastrophic due to its dramatic presentation and because we never pinpoint the etiology. People tend to be deathly ill and almost any virus can lead to this cardiac manifestation. Most of the time, short of giant cell myocarditis, there really is not much to do. Having said that, the long-term outcomes of these patients tends to be counterintuitive to the dramatic presentation.
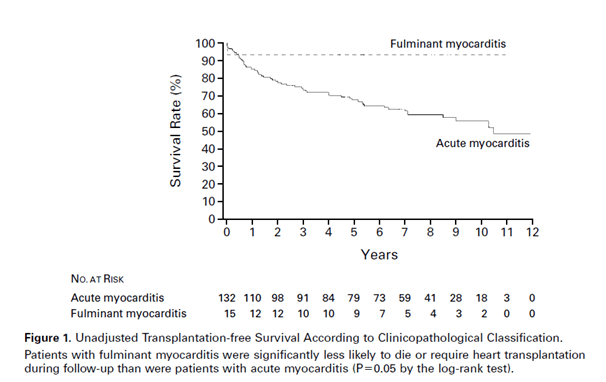
One of the early prospective studies (1) evaluated 15 patients with fulminant myocarditis and 132 with acute myocarditis. Those with fulminant myocarditis required mechanical or inotropic support. End point here was death or heart transplant. Comparing fulminant and acute myocarditis, those with fulminant myocarditis had significantly better outcomes than those with acute myocarditis:
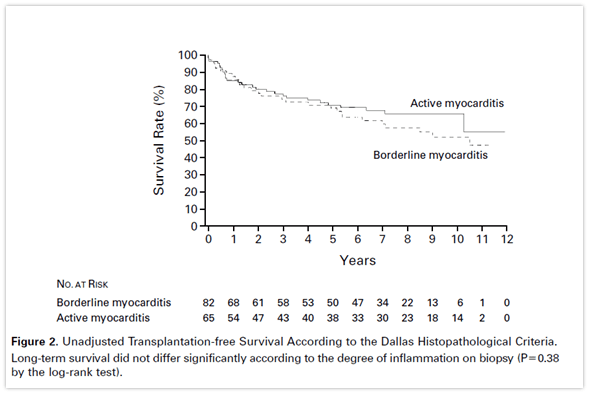
Evaluating pathological diagnosis and survival rate, those with borderline myocarditis (no necrosis) and active myocarditis (+necrosis) had similar rates of survival:
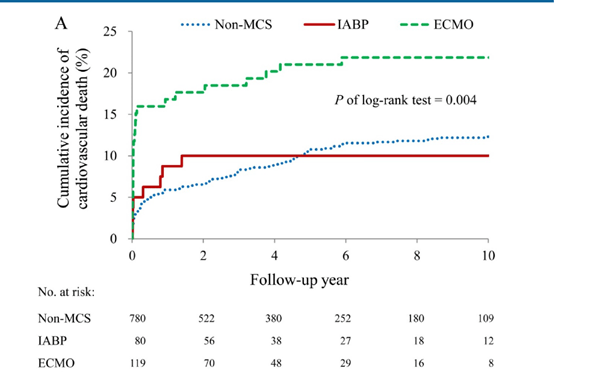
A population based cohort evaluated the long-term outcomes of acute myocarditis in those requiring mechanical support and those that did not (2). Interestingly, this study only included ICU patients. Outcomes were a composite of cardiovascular death, heart failure hospitalization, and all-cause mortality. The incidence of CV death was similar for those with IABP and without mechanical support, though those with ECMO fared worse:
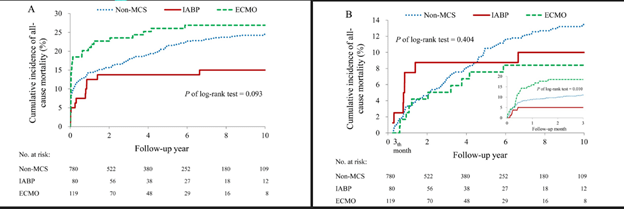
Composite outcome of CV death after 3 months seems to have tapered off for all groups:

The difference in all cause mortality among all groups was not statistically significant, though they tended to favor the IABP group. Mortality within 3 months actually favored the ECMO group, though this difference tapered off after 3 months:
A retrospective study of 55 patients with fulminant myocarditis and 132 with non-fulminant myocarditis evaluated the overall and transplant free survival and EF at discharge and at follow up (3). They found that overall survival was survival was better for non-fulminant myocarditis for all etiologies, but those with fulminant myocarditis from viral etiologies actually did better than expected:
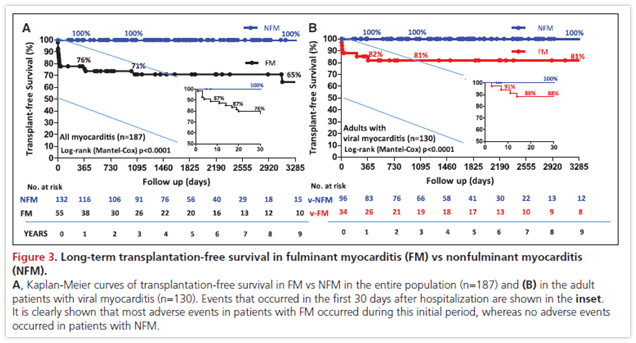
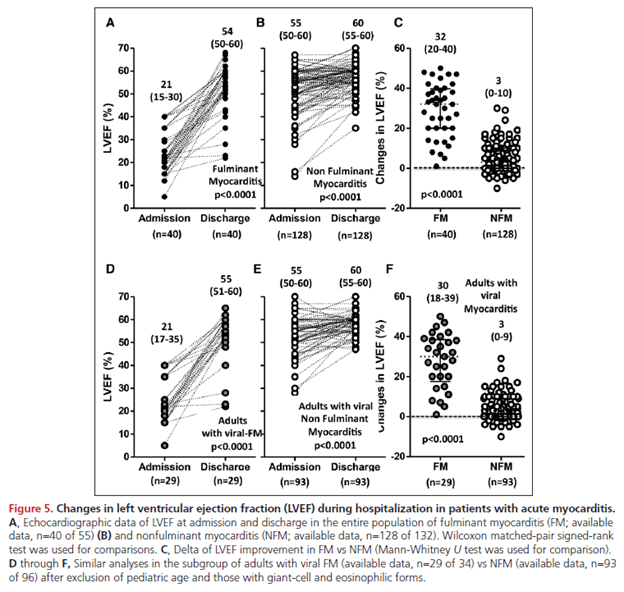
Further, the ejection fraction in fulminant myocarditis tended to recover to near normal levels in both groups, with the fulminant group having a significant rise in the EF:
In a follow up to the above study (4), a retrospective multicenter study was carried out with 2 similar groups, fulminant and non-fulminant myocarditis. Like the above study, primary end point was incidence of cardiac death and transplantation. Not surprisingly, those with uncomplicated presentation did better, with an overall mortality at 5 years of 4.1%, however a 14.7% composite outcome is not terrible in those with a complicated presentation:
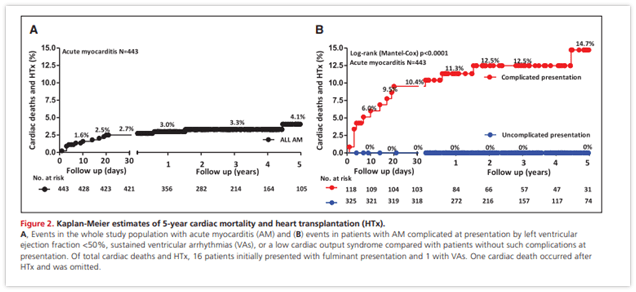
Further, both groups tended to recover their EF quite nicely:

This is reassuring: those with acute fulminant myocarditis will be deathly ill, but the mortality overall does not seem to be as severe as one may think given the degree of illness. 10-20% mortality overall is much better than one would anticipate for someone who ends up on mechanical support with ECMO or Impella devices. The other thing to note is many of these patients tend to recover their ejection fractions at the end of follow up.
What therapies can be offered?
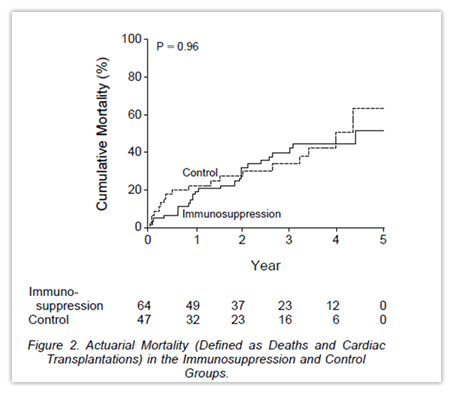
Usually therapy tends to be some sort of immunosuppression or immunomodulator. An old NEJM RCT (5) evaluated 2 groups, either immunosuppression (either azathioprine Or cyclosporine plus prednisone) or none. Therapy was given for 24 weeks and primary outcome was change in EF at week 28. Overall outcomes were not terribly impressive:
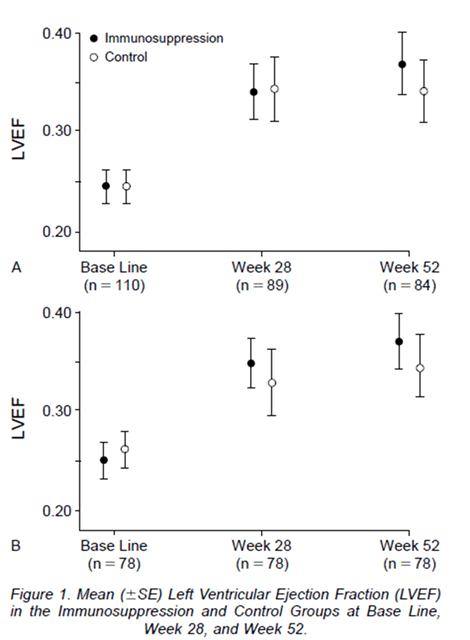
Further, mortality was not significantly different in either group:
A retrospective study (6) evaluated the utility of IVIG on cardiac function and rhythm in fulminant myocarditis. Doses of 400mg/kg/d for 5 days were used. Notably, those who got IVIG tended to be much sicker, with more having cardiogenic shock, renal failure, and required IABP, though this difference was not statistically significant and the EF of both groups was fairly similar.
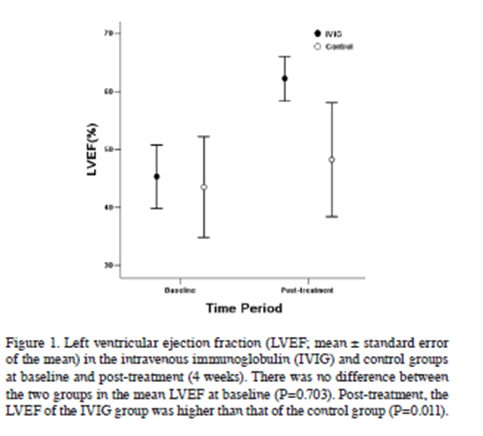
Looking at this, the group with IVIG had significant changes in their EF. Further, the IVIG group had significant reductions in arrhythmias:
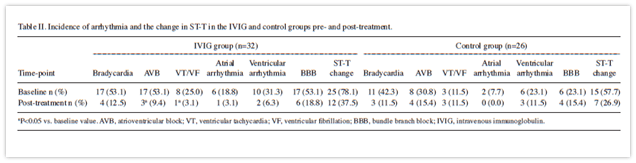
Having said that, there seems to be some bias in this study given its retrospective nature and the tendency for sicker patients to get IVIG, but given their recovery, this bodes well for IVIG as a potential therapeutic agent.
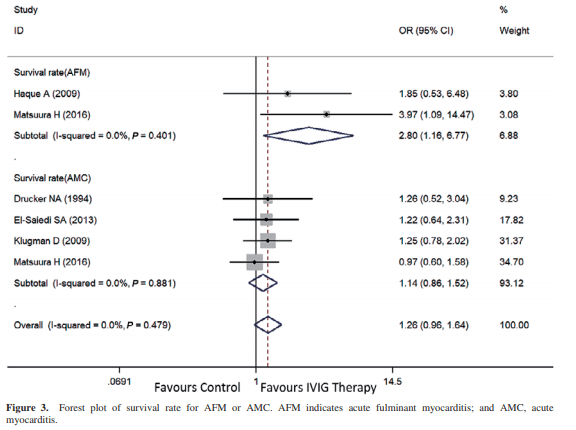
A meta-analysis (7) showed that in myocarditis, IVIG therapy is associated with improved in-hospital mortality:
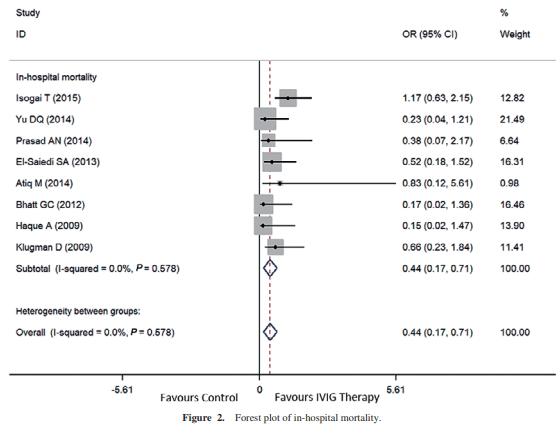
Those with acute fulminant myocarditis tended to benefit more from IVIG when compared to those with acute myocarditis:
But the biggest benefit here seemed to be in terms of improving LVEF when compared to baseline:

The one caveat here is that most of the studies were in pediatrics, however given the overall younger age of presentation of adults with myocarditis, it may be reasonable to generalize until better data becomes available.
What about anti-viral therapy?
A randomized double blind placebo controlled trial evaluated IFN-beta treatment on viral clearance from myocardium and symptomatic relief (7) in chronic viral cardiomyopathy (>6mo with symptoms of heart failure). Those who entered the trial were screened with an endomyocardial biopsy and needed to be positive via PCR for adenovirus, enterovirus, or parvovirus. Patients were assessed for symptoms and repeat biopsy. Patients were evaluated according to different strata (entero/adenovirus and parvovirus). While there was a significant improvement in the adeno/enterovirus strata at week 12, the benefit did not extend beyond this time period:
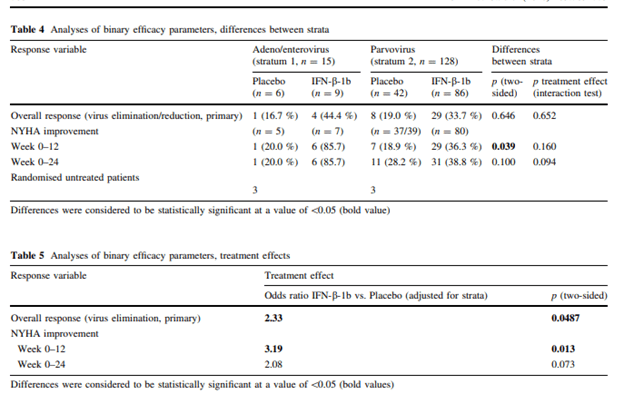
Overall, seems most of the benefit was gained within the first 12 weeks, though there was a trend towards therapy beyond this time frame. Given the low number of patients ,the single center nature of the study, and the chronicity of the illness, it is unclear how this can be useful to the more “critically ill” presentations that are typically seen in patient.
TL;DR
- Fulminant myocarditis tends to have a better outcome than people realize; in other words, throw the kitchen sink at these patients and just wait it out
- There is questionable role for immunosuppressives or antivirals, though IVIG seems to be a reasonable option for some
- Endomyocardial biopsy should be done to rule out giant cell myocarditis ,which benefits from steroids.
References:
- McCarthy RE 3rd, Boehmer JP, Hruban RH, et al. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J Med. 2000;342(10):690-695. doi:10.1056/NEJM200003093421003
- Chang JJ, Lin MS, Chen TH, et al. Heart Failure and Mortality of Adult Survivors from Acute Myocarditis Requiring Intensive Care Treatment – A Nationwide Cohort Study. Int J Med Sci. 2017;14(12):1241-1250. Published 2017 Sep 20. doi:10.7150/ijms.20618
- Ammirati E, Cipriani M, Lilliu M, et al. Survival and Left Ventricular Function Changes in Fulminant Versus Nonfulminant Acute Myocarditis. Circulation. 2017;136(6):529-545. doi:10.1161/CIRCULATIONAHA.117.026386
- Ammirati E, Cipriani M, Moro C, et al. Clinical Presentation and Outcome in a Contemporary Cohort of Patients With Acute Myocarditis: Multicenter Lombardy Registry. Circulation. 2018;138(11):1088-1099. doi:10.1161/CIRCULATIONAHA.118.035319
- Mason JW, O’Connell JB, Herskowitz A, et al. A clinical trial of immunosuppressive therapy for myocarditis. The Myocarditis Treatment Trial Investigators. N Engl J Med. 1995;333(5):269-275. doi:10.1056/NEJM199508033330501
- Yu DQ, Wang Y, Ma GZ, et al. Intravenous immunoglobulin in the therapy of adult acute fulminant myocarditis: A retrospective study. Exp Ther Med. 2014;7(1):97-102. doi:10.3892/etm.2013.1372
- Huang X, Sun Y, Su G, Li Y, Shuai X. Intravenous Immunoglobulin Therapy for Acute Myocarditis in Children and Adults. Int Heart J. 2019;60(2):359-365. doi:10.1536/ihj.18-299
- Schultheiss HP, Piper C, Sowade O, et al. Betaferon in chronic viral cardiomyopathy (BICC) trial: Effects of interferon-β treatment in patients with chronic viral cardiomyopathy. Clin Res Cardiol. 2016;105(9):763-773. doi:10.1007/s00392-016-0986-9
