This is a confusing bit that no one really seems to understand, because it seems so basic. Bactericidal antibiotics kill bacteria, bacteriostatic doesn’t. Seem simple, but it’s a bit more complicated.
First things first: all antibiotics kill. Otherwise, they wouldn’t work. The whole bacteriocidal vs static definition is mostly a microbiogical one rather than a clinical one. In other words, the definitions come from the microbiology lab, in a more controlled setting, than anything that happens in the body.
The TL;DR if you know your stuff is as follows: it is the ratio between MBC/MIC aka minimum bacteriocidal concentration/minimum inhibitory concentration.
- IF ratio >4 (i.e. 32/4) = bacteriostatic. You can conceptualize this as you requiring 4 times as much antibiotic to get from “stunting” growth to “kill” bacteria (again, not what happens)
- If ratio <4 (i.e. 2/1 ) = bactericidal. You do not need to jump “that high” of a concentration to start killing bacteria
Of course, this is not what happens. They all kill bacteria, but it is the rate at which they kill bacteria that defines bacteriostatic vs cidal. One review states that “those agents that are called bacteriocidal usually fail to kill every organism (if for instance, the inoculum is large) within 18-24h after the test, and most so-called “bacteriostatic” agents kill some bacteria…often more than 90-99%….but not enough to be called bactericidal”
The in vitro microbiological determination of whether an antibacterial agent is bactericidal or bacteriostatic may be influenced by growth conditions, bacterial density, test duration, and extent of reduction in bacterial numbers
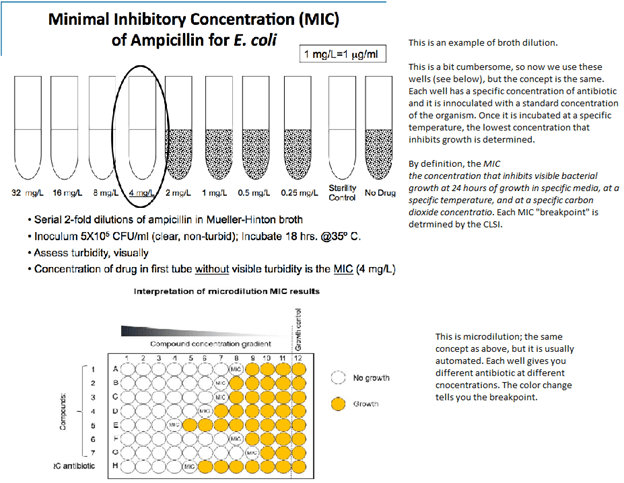
A bit on susceptibility testing. There are 2 methods to do this: dilution and diffusion
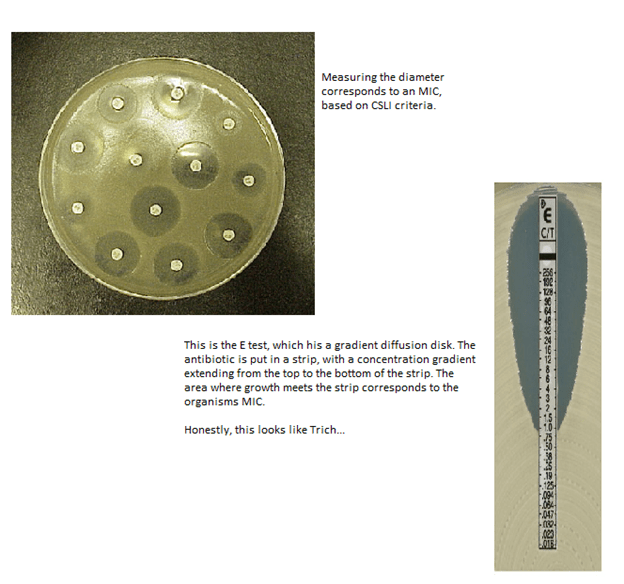
Diffusion method: just like it sounds like. An agar test plate is swabbed with a standard concentration of the test organism, and then appear disks containing a defined antibiotic concentration are placed on the lawn of bacteria. The disk is left to incubate overnight and the diameter of the zone of inhibited growth around the disc is measured. This zone is influenced by lots of variables (test medium, agar, concentration of the organism, concentration of antibiotic, etc)
TL;DR – the above methods measure the minimum inhibitory concentration. In other words, MIC = concentration of antibiotic that inhibits bacterial growth at 24 hours in a specific media, at a specific temperature. So this is the number that we clinically use. So how do we calculate MBC?

In other words, the bactericidal vs -static is a microbiological definition, that depends largely on the medium, temperature as well the concentration of antibiotic used in testing. The clinical implications here are unclear. For instance, there are situations (depending on the clinical context), where a “bacteriostatic” antibiotic may actually have “bactericidal” properties (i.e. macrolides being -static but being bactericidal against strep pneumo).
Traditionally, it has been believed that for diseases such as endocarditis (where there is fibrin, clot and other things involved that make it more difficult for antibiotic to penetrate), you would opt for a bactericidal antibiotic (with the idea being you only need a bit of higher concentration for more efficient killing.) This is also because the concentrations of bacteria within an infected valve may be so high and dense, the rate of metabolism and cell division drops leading to a “decreased efficacy” of cell active agents (aka the “Eagle effect.”). Whether or not this is true is difficult to say, however this may explain the better outcomes seen in MSSA an anti-staph beta lactam vs the traditional “-cidal” agent, vancomycin.
For other infections such as SSTI or pneumonia, a recent review (doi:10.1093/cid/cix1127) did not find any data suggesting the use of bactericidal over -static agents. Another review did not find any evidence for the use of bacteriocidal over static agents in intra-abdominal infections (. https://doi.org/10.1093/jac/dku379). All in all, the clinical significance of this distinction may not matter, but more data on more serious infections such as meningitis and endocarditis is needed.
TL;DR
- All antibiotics kill bacteria. The distinction of -cidal vs -static is a microbiological definition that depends on many variables (ratio of MBC/MIC)
- The clinical significance of this distinction may not matter much, with the exception of possibly endocarditis.
- There is no evidence of the superiority of bactericidal antibiotics over bacteriostatic antibiotic for pneumonia, SSTI, and other non-serious infection.
References:
Johannes Nemeth, Gabriela Oesch, Stefan P. Kuster, Bacteriostatic versus bactericidal antibiotics for patients with serious bacterial infections: systematic review and meta-analysis, Journal of Antimicrobial Chemotherapy, Volume 70, Issue 2, February 2015, Pages 382–395, https://doi.org/10.1093/jac/dku379
Pankey, G A., and L D. Sabath. “Clinical Relevance of Bacteriostatic Versus Bactericidal Mechanisms of Action in the Treatment of Gram-positive Bacterial Infections.” Clinical Infectious Diseases : an Official Publication of the Infectious Diseases Society of America, vol. 38, no. 6, 2004, pp. 864-70.
Wald-Dickler, Noah, et al. “Busting the Myth of “Static Vs Cidal”: a Systemic Literature Review.” Clinical Infectious Diseases : an Official Publication of the Infectious Diseases Society of America, vol. 66, no. 9, 2018, pp. 1470-1474.

3 comments on “Bacteriostatic vs Bactericidal”